"In half of Spain there is no palliative care. What kind of decision is the patient going to make when the law says that palliative care must be explained to him or her?
What is he going to choose between?" asked Dr. Marcos Gómez Sancho, who began working in Palliative Medicine as early as 1989, with the creation of a specialized Unit at the Hospital de Gran Canaria Dr. Negrín, and who currently coordinates the Observatory of Medical Care at the End of Life of the Council of Medical Associations.
The palliative expert pointed out that there are basically two groups of patients who are possible candidates for requesting euthanasia. "Oncology patients and similar patients in advanced or terminal stages, and the chronically ill, elderly people with disabling diseases, who require a model of residential socio-health care. Both situations are scandalously deficient in Spain. Today we know that approximately 75,000 Spanish patients die each year with intense suffering because they do not have access to palliative care. And that is something that should not be allowed," he said.
"The other group of patients who may be candidates to request euthanasia are the elderly patients with chronic, degenerative and evolutive, disabling diseases, who need social-health centers to be cared for.
Well, they should know that Spain lacks 71,000 beds of this type, which is an understatement".
At this point, the doctor made an aside to specify that "there are economic problems. According to the spokesman for the Luzon Foundation, which studies and helps patients with Amyotrophic Lateral Sclerosis (ALS), 94 percent of the patients do not have the resources to be able to privately finance the care they need.
So, if there is no access to a public residential place, because there are 71,000 beds missing, and only 6 percent can afford a private one, it is clear what the situation is."
Because "every day 160 sick people die waiting, in a sinister waiting list, for the dependency assistance to which they are entitled, because they have already been evaluated and have been granted".
His conclusion, placing the context in the recent entry into force of the euthanasia law, is "that we should have started there; that is, by developing palliative care, so that there are not 75,000 patients who die every year with intense suffering because they do not have access to palliative care. And that there should be sufficient social and health centers so that these chronic patients, with degenerative diseases, can be adequately cared for".
"What was urgent was not to legalize the way to end a sick person's life," he stressed, "but that no one should have to wait ten years for the resources they need to be put in their hands, and that they should not have to be forced to end their life or to ask their husband or wife to end it. This is the first thing that should have been done, before developing a law on euthanasia".
Palliative Sedation Guide 2021
In any case, the Consejo General de Colegios Oficiales de Médicos and the Sociedad Española de Cuidados Paliativos have today provided a medical solution to intense suffering, that is, a Palliative Sedation Guide 2021This document is intended to serve as a guide for good practice and for the correct application of palliative sedation.
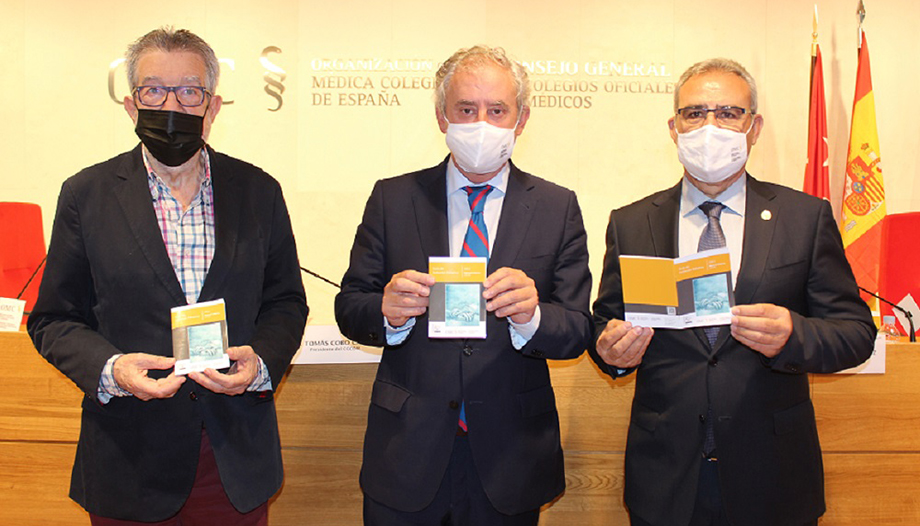
"This text is born at a crucial moment, and it plays an essential role, which is the one that must be played by the General Council of Medical Associations of Spain (CGCOM), and is to provide and generate tools that are truly useful in daily healthcare practice," said Dr. Tomás Cobo Castro, president of the CGCOM.
"This Palliative Sedation Guide is precisely that, a tremendously practical, direct tool that sets out protocols and the use of certain drugs [medications] in palliative sedation," added Dr. Cobo Castro, who was accompanied by the Secretary General, Dr. José María Rodríguez Vicent, and Dr. Marcos Gómez Sancho. The guide has been drawn up by the Observatory of Medical Care at the End of Life of the CGCOM, and SECPALThe new publication, which highlights palliative sedation as a good medical practice, can be downloaded through the CGCOM website and the QR code to carry it with you at all times.
"Sedation, very different from euthanasia."
"There are people who confuse palliative sedation with euthanasia, and it is not at all the same thing, not even similar," Dr. Gómez Sancho began by explaining. "They are differentiated by several things. First, the intention. The intention of palliative sedation is to alleviate the suffering of the patient, while the intention of euthanasia is to end the patient's life."
"The drugs used are also different. In palliative sedation, benzodiazepines are used first and almost always, specifically midazolam,
Sometimes, in cases of hyperactive delirium, other drugs, including barbiturates, must be used. However, in the case of euthanasia, barbiturates are used directly.
"The procedure is also different. In palliative sedation, the minimum doses are used to achieve our objective, which is to reduce the patient's consciousness, so that he or she does not suffer. However, in the case of euthanasia, directly lethal doses are used."
"And then the result. The result of palliative sedation is a sedated patient, asleep, not suffering. The result of euthanasia is a dead man. There is also survival. In the case of palliative sedation, it can be hours, and even some small number of days. In the case of euthanasia it is a few minutes, three, four, five minutes."
"Therefore," concludes the prestigious palliativist, "one thing is quite different from the other. Although it is true that what separates them is a very fine line, it is a perfectly clear line, and it differentiates very clearly between what is a medical act and what is a euthanasic act. Palliative sedation is a tool that should be known by all Spanish doctors, because there is practically no doctor who does not have to attend at some point in his professional career to a patient at the end of his life. And he or she must know that this treatment exists, and must know how to apply it perfectly".
"That is why I congratulate the OMC [Organización Médica Colegial], for having published this pocket guide, because with it no doctor can say that he does not know how to do it, because it is perfectly clear and detailed when and how a doctor has to perform palliative sedation on his patient".
Half of the patients need it
"The guide explains in detail the steps to follow for palliative sedation," Dr. Gómez Sancho added. "Palliative sedation in children, in pediatrics, has also been added, as well as palliative sedation in cases of refractory existential suffering. It is an extraordinarily important document, so that it can reach all Spanish physicians, residents, medical students, etc.
In his opinion, "it is an essential resource today to face the end of life of our patients, because we believe that between 50 and 60 percent of patients at the end of life will need palliative sedation, to have a peaceful, dignified end, and at the right time.
"It is very important," he added, "because with this treatment, with palliative sedation, there should be no need for any other type of action with any patient at the end of life. Because with perfect palliative sedation, strictly and rigorously applied, no person has to die in pain or with any other stressful symptom."
"Therefore, I think that's where things should have started, because in this way, as I say, we would avoid that no person is going to die with intense suffering, caused by one or more particularly stressful symptoms."
In addition, the doctor assured, "palliative sedation must be applied when the patient needs it. Obviously, we have to evaluate each patient individually, and if a patient is in need of palliative sedation, we do not have to pay too much attention to how much time this patient has left to live, but rather apply the treatment at the moment he or she needs it.
Demand for palliative care law
During question time, "the president of the WTO, Dr. Cobo Castro, acknowledged that "we have been bored of asking for a law on Palliative Care, and we have also been bored of asking, when the law on euthanasia was drafted, that they should have counted more on healthcare professionals".
Dr. Gómez Sancho confirmed this fact, and assured that "the demand for a palliative care law has been made persistently by this house. And we have also done so from the Spanish Society of Palliative Care, and from the Observatory itself".
The palliative physician added that "the request has not been heeded so far by any political party. We have been trying for more than 30 years to have a Palliative Care Law. This is a warning to all political parties, because in these thirty-odd years, all political parties have passed through the Ministry of Health and have ignored our proposal. Because the priority is not a law on euthanasia. The priority should have been to make a law to care for the sick so that they do not have to request euthanasia. Because we have started the house from the roof".